Type 1 Diabetes Stem Cell Therapy: A Promising Approach for Managing Autoimmune Diabetes
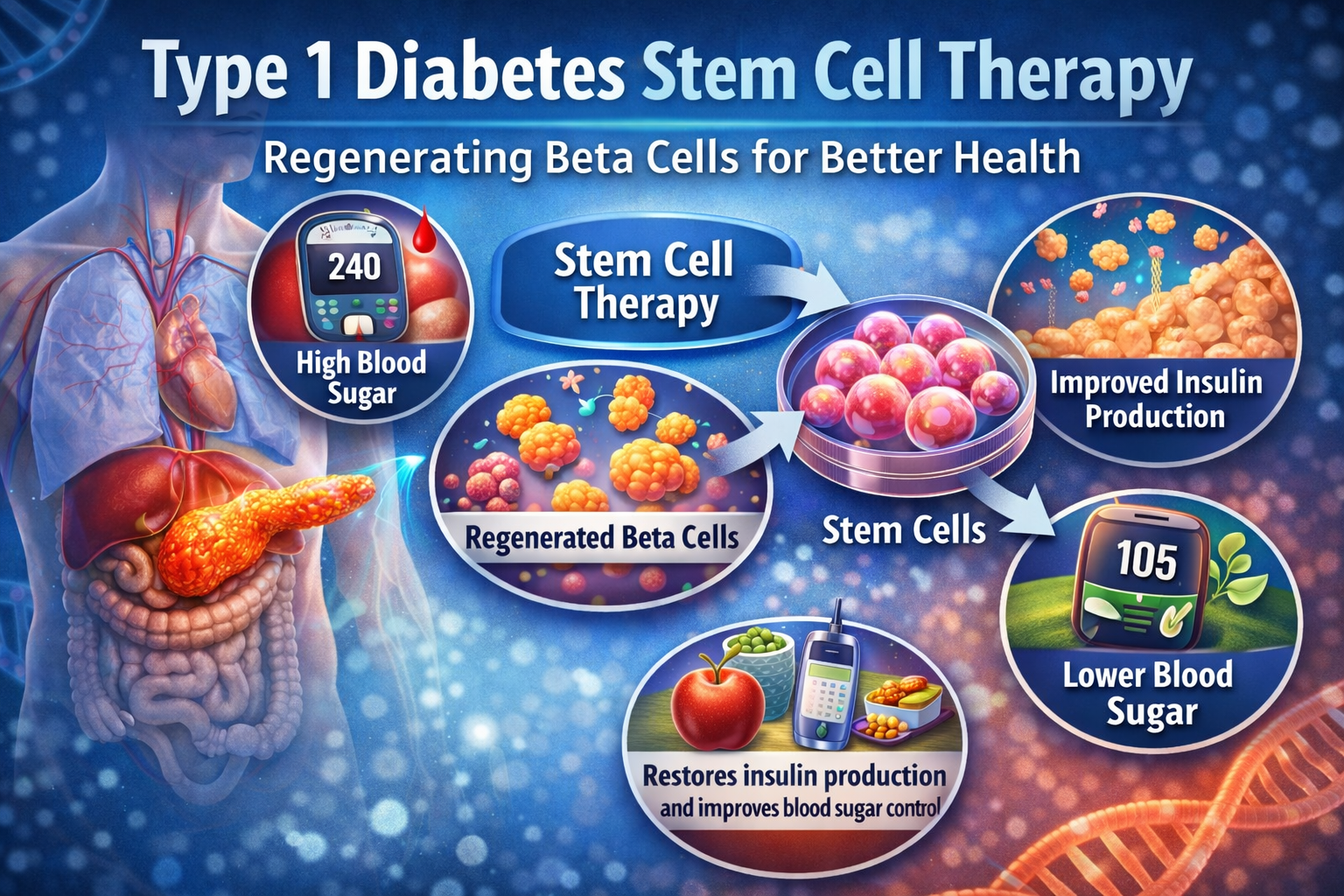
Type 1 diabetes is a chronic autoimmune disorder in which the body’s immune system attacks insulin-producing beta cells in the pancreas. This results in little to no insulin production, leading to elevated blood glucose levels, or hyperglycemia. Traditional management of type 1 diabetes relies on daily insulin injections, glucose monitoring, and lifestyle modifications. While these measures help regulate blood sugar, they do not address the underlying autoimmune destruction of beta cells. This is where Type 1 Diabetes Stem Cell Therapy is emerging as a revolutionary treatment option, aiming to restore pancreatic function and improve the quality of life for patients.
Understanding Type 1 Diabetes
In type 1 diabetes, the immune system mistakenly identifies pancreatic beta cells as foreign and destroys them. These beta cells are crucial for producing insulin, the hormone responsible for regulating blood sugar levels. Without sufficient insulin, glucose accumulates in the bloodstream, causing various complications including nerve damage, kidney disease, vision problems, and cardiovascular disorders. Current therapies manage symptoms but cannot reverse the autoimmune process or regenerate lost beta cells.
What is Stem Cell Therapy?
Stem cells are unique cells with the ability to differentiate into various specialized cell types in the body. They also possess self-renewal capabilities, meaning they can replicate to produce more stem cells. These characteristics make stem cells a valuable tool for regenerative medicine. Type 1 Diabetes Stem Cell Therapy involves using stem cells to repair or replace damaged pancreatic beta cells, potentially restoring insulin production and reducing dependence on exogenous insulin.
How Stem Cell Therapy Works in Type 1 Diabetes
Stem cell therapy for type 1 diabetes primarily focuses on three approaches:
Autologous Stem Cell Transplantation: In this method, stem cells are harvested from the patient’s own bone marrow or blood. These stem cells are processed and reintroduced into the body to stimulate regeneration of beta cells. Using the patient’s own cells reduces the risk of immune rejection.
Allogeneic Stem Cell Transplantation: Stem cells are sourced from a donor, often umbilical cord blood or bone marrow. These cells are used to replace or repair damaged beta cells. Immunosuppressive therapy is often required to prevent rejection by the recipient’s immune system.
Differentiated Beta-like Cells from Pluripotent Stem Cells: Researchers are developing techniques to transform pluripotent stem cells into functional beta-like cells. These cells can be transplanted into the patient, where they ideally integrate with existing pancreatic tissue and restore insulin production.
Potential Benefits of Stem Cell Therapy for Type 1 Diabetes
The goal of Type 1 Diabetes Stem Cell Therapy is not just symptom management but functional cure or remission. Some potential benefits include:
Restoration of Insulin Production: By regenerating beta cells, stem cell therapy can enable the pancreas to produce insulin naturally, reducing or eliminating the need for insulin injections.
Improved Blood Sugar Control: Restored beta cell function can lead to more stable glucose levels, minimizing fluctuations and reducing the risk of complications.
Delay or Prevention of Diabetes Complications: Better glucose regulation helps protect organs and tissues from damage caused by prolonged hyperglycemia.
Reduced Dependence on Exogenous Insulin: Patients may experience fewer daily injections, improving their quality of life.
Challenges and Risks
Despite its promise, stem cell therapy for type 1 diabetes faces several challenges:
Immune System Attacks: Since type 1 diabetes is autoimmune in nature, newly introduced beta cells may also be targeted by the immune system. Immunomodulatory strategies are required to protect these cells.
Risk of Tumor Formation: Stem cells have the potential to proliferate uncontrollably if not properly controlled, posing a risk of tumor development.
Cost and Accessibility: Stem cell therapy is an advanced treatment that may not be widely available and can be expensive.
Long-Term Efficacy: Clinical studies are still ongoing to determine how long the benefits of stem cell therapy last and whether repeated treatments are needed.
Current Research and Clinical Trials
Research in Type 1 Diabetes Stem Cell Therapy is advancing rapidly. Clinical trials have tested autologous hematopoietic stem cell transplantation (HSCT) to reset the immune system and regenerate beta cells. Some patients have experienced temporary insulin independence and improved glucose control. Additionally, scientists are exploring the use of induced pluripotent stem cells (iPSCs) to generate beta-like cells that are less susceptible to immune attacks.
Future Prospects
The future of Type 1 Diabetes Stem Cell Therapy is highly promising. Advances in genetic engineering, immunomodulation, and tissue engineering may overcome current limitations. Combining stem cell therapy with immunotherapy could provide a long-lasting solution, protecting regenerated beta cells from autoimmune destruction. Researchers are also investigating encapsulation techniques to shield transplanted cells from immune attacks while allowing them to release insulin effectively.
Conclusion
Type 1 Diabetes Stem Cell Therapy represents a groundbreaking approach in the treatment of autoimmune diabetes. By addressing the root cause—the loss of insulin-producing beta cells—this therapy offers hope for improved glucose control, reduced insulin dependence, and potentially long-term remission. While challenges remain, ongoing research and clinical trials are steadily advancing toward making this therapy a viable option for patients worldwide. With continued innovation, stem cell therapy could transform the management of type 1 diabetes, offering a path toward a functional cure.